FECAL TRANSPLANTS and how they could cure IBD.
While this guide discusses home-based fecal transplants, the opinion of Crohnsforum.com is that they should be done under the supervision of a trained clinician as fecal transplants are potentially dangerous. ALWAYS discuss any potential treatment with your doctor. - Forum Admin
Fecal Microbiota Transplants(FMT) have induced sustained drug free remissions in both forms of Inflammatory Bowel Disease(IBD) and may have cured some cases of IBD in small trials, according to Gastroenterologist Doctor Thomas J. Borody MD, Ph.d. Details of these reports are listed in section 1.
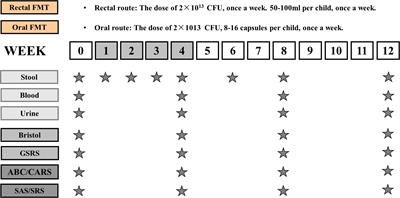
There are 14 F.D.A clinical trials planned for the use of fecal transplant in both forms of IBD. In this post you will find out everything about them. Fecal transplants restore missing bacteria in IBD patients by obtaining them from healthy donors stool, mixing a stool sample with saline solution in a blender and giving it to the patient as an enema. This procedure has been performed successfully at home, but if your decide to do it, be sure to read the papers in the post below for expert instruction, don't just jump into it, donors need to be absolutely healthy.
http://www.cghjournal.org/article/S1542-3565(10)00069-8/fulltext
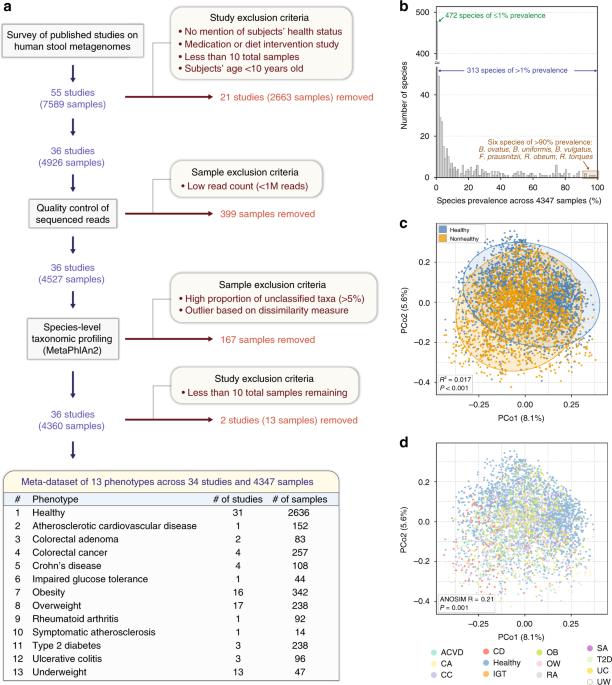
Latest studies in IBD show reduced diversity of healthy bacteria that regulate the inflammatory response when compared to groups of healthy people without IBD. Therefore, it is believed by some scientists that the restoration of the bacteria in IBD patients will correct the abnormal inflammatory response. So far we have some good scientific evidence this may be the case, but it will take time to prove this theory with absolute certainty. With official reports of UC and Crohn's patients maintaining a drug free remissions for as long as 25 and 13 years, this provides some compelling supportive evidence that they may have been cured by FMT.
Other ways of performing a fecal transplant are orally through a nasogastric/duodenal/jujenal tube or pill form which is currently in development. So far the studies have shown
when donors are well screened with blood tests and meet health criteria, this is generally a safe treatment.
My experiences with Fecal Transplants: In this thread i have posts which detail my experiances with FMT, I was trying to find a way to make a FMT pill which proved pretty difficult. I tried FMT 4x with 3 different donors, only one FMT led to improvements, such as gaining 10 pounds in 10 weeks, improved bowel movements, lowered anxiety, but the majority of my other symptoms remain so I will have to find a new donor and try it again, but I'm convinced doing this again will likely reduce the severity of my disease even more.
----Receive updates and notifications from this thread by subscribing via the upper right menu labeled THREAD TOOLS.----
Outline
1. History of Fecal Transplant in IBD: Its success so far
2. Clinical Studies Currently in progress
3. Testimonies.
4. General Information
5. How to select a Donor
6. How to perform a Fecal Transplant
------------------------------------
1. History of Fecal Transplants in IBD: Its Success So Far.
Dr. Borody Background
These studies were done by a doctor in Australia, Thomas J. Borody who is trained in Gastroenterology in addition to other education and experience in scientific research.
Educational/Career background on Doctor Borody.
BSc (MED) (HONS)(Bachelor of Science), MBBS (HONS)(Bachelor of medicine, Bachelor of Surgery), MD(Doctor of Medicine), PhD(Doctor of Philosophy), FRACP(Fellow of the Royal Australasian College of Physicians), FACG (Fellow of the American College of Gastroenterology), FACP (A Fellow in the American College of Physicians), AGAF (American Gastroenterology Association Fellow)
Link to his website where this information was derived-
http://www.cdd.com.au/pages/clinical_staff.html
Here is a link to the U.S. National Library of Medicine /National Institute of Health where a search on his name will show some of his published contributions to various Medical/Scientific journals, search results on this database reveal 74 references to his name which illustrate more documentation of his professional experience. These references date from as recent as 2013 to as far back 1979, spanning about 34 years.
http://www.ncbi.nlm.nih.gov/pubmed/?term=borody+t
Fecal Transplant Studies on IBD -
1989 – Doctor Borody first used fecal transplants in 55 patients with a wide range of Gastrointestinal disorders ranging from constipation, diarrhea of unknown cause, Crohn’s disease and ulcerative colitis. 20 were considered cured. 9 were improved and 26 were unchanged. At least one of the cured patients were cured of Crohn’s disease and one of ulcerative colitis. This is an early study so it was unknown how many times a transplant may have to be done to get any results.
http://www.cdd.com.au/pdf/publications/All Publications/1989-Bowel-flora alteration a potential cure for inflammatory bowel disease and irritable bowel syndrome, Med J Aust, vol 150, issue 10 p604.pdf
2003- Doctor T.J Borody tried this therapy on 6 patients with ulcerative colitis, that elimated all signs of disease symptoms without drugs ranging from 1-13 years after therapy. These patients are considered to be potentially cured since there is no sign of disease, no longer need medication beyond 2 years and they remain disease free to this day. This study was published in the journal of clinical gastroenterology.
http://prdupl02.ynet.co.il/ForumFiles_2/28701499.pdf
2011- The same researcher Dr borody reported results in a group of patients with Crohn’s disease and all patients obtained remission without drugs. These were severe cases that didn’t respond to any medication before doing the fecal transplant. The results and details of this study were presented at the American College of Gastroenterology’s (ACG) 76th Annual Scientific meeting in Washington, DC in November of 2011. Here is the Official news release from the American college of gastroenterology-
http://d2j7fjepcxuj0a.cloudfront.ne...2011acg_fecal-transplant-cdiff_FINAL_1025.pdf
references for the 2011 fecal transplant study on crohn’s
Some reports of the ACG meeting in 2011 on various news websites
http://www.medicalnewstoday.com/releases/236885.php
http://www.sciencedaily.com/releases/2011/10/111031114945.htm
2013
July- 14 year old boy with crohns achieves remission with FMT -http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3742951/?report=classic
September- Early results from the mcmaster study, news segment-
http://www.ctvnews.ca/health/experi...tionize-treatment-of-bowel-diseases-1.1445800
November - man with severe crohn's disease achieves complete remission without drugs and with only one fecal transplant delivered orally.
http://www.ncbi.nlm.nih.gov/pubmed/24222969?dopt=Abstract
November- patient with crohn's responds to fecal transplant
http://www.ncbi.nlm.nih.gov/pubmed/24239403
FULL TEXT
http://ecco-jcc.oxfordjournals.org/content/8/3/256
2014
March- Woman remains in remission for 13 years after recieving an oral fecal transplant for Crohns disease, she may have been cured.
http://www.abc.net.au/news/2014-03-18/sydney-doctor-claims-poo-transplants-curing-diseases/5329836
additional source:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3868025/
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3868025/figure/F2/
May-Mcmaster Ulcerative Colitis Study.
Mixed results, some bad responses while some very good responses to FMT.
http://www.medscape.com/viewarticle/824930
August - Beth Israel deaconess Medical center Crohn's Disease,
After 4 weeks of follow-up, 55% had clinical response; 36% were in clinical remission.
http://www.healio.com/gastroenterology/inflammatory-bowel-disease/news/online/{13d3a6cd-6dde-4871-b904-21770537217d}/fecal-microbiota-transplant-improved-symptoms-in-patients-with-crohns-disease
2015
January-Crohn's- 23 out of 30 patients achieve remission with one oral administration of Fecal Transplant.
http://www.ncbi.nlm.nih.gov/pubmed/25168749
March-Crohn's-
http://journals.lww.com/ibdjournal/...icrobial_Transplant_Effect_on_Clinical.7.aspx
Fecal Transplant History of use for C. Difficle Infection.
Here are some reports about the latest study on Fecal Transplants outperforming standard Antibiotic therapy for C. Diff.-
http://www.cbsnews.com/8301-204_162...cs-for-curing-diarrhea-caused-by-c-difficile/
Here is a link to the actual study published in the New England journal of medicine 2013
http://www.nejm.org/doi/full/10.1056/NEJMoa1205037#t=abstract
EXCERPT from the study-
“The study was stopped after an interim analysis. Of 16 patients in the infusion group, 13 (81%) had resolution of C. difficile–associated diarrhea after the first infusion. The 3 remaining patients received a second infusion with feces from a different donor, with resolution in 2 patients. Resolution of C. difficile infection occurred in 4 of 13 patients (31%) receiving vancomycin alone and in 3 of 13 patients (23%) receiving vancomycin with bowel lavage (P<0.001 for both comparisons with the infusion group). No significant differences in adverse events among the three study groups were observed except for mild diarrhea and abdominal cramping in the infusion group(fecal transplant) on the infusion day.
Here is a quote by University of Minnesota Doctor and Researcher Alex Khoruts
some info on him-
http://www.med.umn.edu/gi/faculty/khoruts/
"Those of us who've been doing this procedure(fecal transplant) for some time didn't need any more convincing, but the large medical community needs to go through these steps," Dr. Alexander Khoruts, a gastroenterologist at the University of Minnesota in Minneapolis who was not involved in the new study, told Nature. "It's an unusual situation where we have more than 50 years of worldwide experience and more than 500 published cases, and only this far along does a randomized trial appear.”
link to quote-
http://www.cbsnews.com/8301-204_162...cs-for-curing-diarrhea-caused-by-c-difficile/
2. CLINICAL STUDIES: Currently In Progress
These studies were found on
www.clinicaltrials.gov. To verify their existence, enter the identifier code into the website search engine.
-----------------------------------------
Pediatric Inflammatory Bowel Disease(Ulcerative colitis)
Helen DeVos Childrens Hospital (HDVCH)
Grand Rapids, Michigan, United States, 49503
ClinicalTrials.gov Identifier: NCT01560819
Estimated Primary Completion Date: May 2013
recently released study results April 4, 2013-
http://www.sciencedaily.com/releases/2013/04/130405112859.htm
excerpt-
“Results showed that, 78 percent subjects achieved clinical response within one week while 67 percent subjects maintained clinical response at one month after FMT. Thirty-three percent subjects did not show any symptoms of ulcerative colitis after FMT. Patient's clinical disease activity (PUCAI score) significantly improved after FMT compared to the baseline. No serious adverse events were noted. “Patients often face a tough choice between various medications that have significant side effects. Allowing the disease to progress can lead to surgical removal of their colon," said Dr. Kunde. "Our study showed that fecal enemas were feasible and well-tolerated by children with ulcerative colitis. Adverse events were mild to moderate, acceptable, self-limited, and manageable by patients."
----------------------------------------------------------
Ulcerative Colitis
University of Washington
Seattle, Washington, United States, 98103
ClinicalTrials.gov Identifier: NCT01742754
Estimated Study completion Date: April 2013
------------------------------------------------------------------------
Ulcerative colitis
Academic Medical Center
Amsterdam, Netherlands, 1100DD
ClinicalTrials.gov Identifier: NCT01650038
Estimated study Completion Date: December 2013
------------------------------------------------------------------------
Ulcerative Colitis
Hamilton Health Sciences / McMaster University
Hamilton, Ontario, Canada, L8N 3Z5
ClinicalTrials.gov Identifier: NCT01545908
Estimated Primary Completion Date: March 2014
-----------------------------------------------------------------------
Crohn's Disease
Beth Israel Deaconess Medical Center
Boston, Massachusetts, United States, 02215
ClinicalTrials.gov Identifier: NCT01847170
Estimated Enrollment: 20
Study Start Date: May 2013
Estimated Study Completion Date: April 2014
-------------------------------------------------------------------------
Crohn’s disease and Ulcerative colitis
Seattle Children's Hospital
Seattle, Washington, United States, 98105
ClinicalTrials.gov Identifier: NCT01757964
Estimated Primary Completion Date: December 2014
--------------------------------------------------------------------------
Crohn’s Disease
Medical Center for Digestive Diseases, The Second Affiliated Hospital of Nanjing Medical University
Nanjing, Jiangsu, China, 210011
ClinicalTrials.gov Identifier: NCT01793831
Estimated Study Completion date: December 2014
--------------------------------------------------------------------------
Ulcerative Colitis
Medical Center for Digestive Diseases, The Second Affiliated Hospital of Nanjing Medical University
Nanjing, Jiangsu, China, 210011
ClinicalTrials.gov Identifier: NCT01790061
Estimated Study Completion Date: December 2014
--------------------------------------------------------------------------
Ulcerative Colitis
University of Chicago Medicine Recruiting
Chicago, Illinois, United States, 60637
ClinicalTrials.gov Identifier: NCT02058524
Estimated Enrollment: 20
Study Start Date: June 2013
Estimated Primary Completion Date: June 2015
------------------------------------------------------------------
Ulcerative Colitis
University of South Wales
ClinicalTrials.gov Identifier: NCT01896635
Estimated Enrollment: 80
Study Start Date: September 2013
Estimated Study Completion Date: September 2016
-------------------------------------------------------------------------
Ulcerative Colitis
Texas Children's Hospital/Baylor college of medicine
ClinicalTrials.gov Identifier: NCT01947101
Estimated Enrollment: 10
Study Start Date: December 2013
Estimated Study Completion Date: December 2016
---------------------------------------------------------------------------
Crohn's Disease
Gastroenterology department, Saint Antoine Hospital
Paris, France, 75571
ClinicalTrials.gov Identifier: NCT02097797
Estimated Enrollment: 18
Study Start Date: March 2014
Estimated Study Completion Date: February 2016
------------------------------------------------------
IBD both forms
Department of General Surgery, Jinling hosptal,Medical School of Nanjing University Nanjing, Jiangsu, China, 210002
ClinicalTrials.gov Identifier: NCT02016469
Estimated Enrollment: 30
Study Start Date: December 2013
Estimated Study Completion Date: February 2016
--------------------------------------------
--------------------------------
IBD both forms
Wolfson Medical Center, Holon, Israel.
ClinicalTrials.gov Identifier: NCT02033408
Estimated Enrollment: 20
Study Start Date: January 2014
Estimated Study Completion Date: January 2016
------------------------------------------------
Seattle Children's Hospital, David Suskind.
ClinicalTrials.gov Identifier:NCT02272868
Estimated Enrollment: 32
Study Start Date: October 2014
Estimated Study Completion Date: October 2016
3. TESTIMONIES.
-
Testimony #1
This is the best testimony I have found so far because it is so detailed. This is a guy who used his son and his wife as donors. You don’t have to watch the entire videos, you can skip to the parts I have defined in the summary to verify the story. You will notice in the last video that the energy in his voice changes and his speaking ability improves a bit and his mood seems slightly improved, which are signs his health has is improving due to the fecal transplants.
Video #1 –
video length- 33 minutes
Summary of video/skip to these parts-
2:52- 30 years old, Married for 8 years, Bachelors degree in Business Adminstration, Self Employed, Works in financial services industry, Healthy most of life. Has had ulcerative colitis for about 5 years.
7:20- Took antibiotics for 2 years for staph infections on legs, he suspects the antibiotics had something to do with his development of IBD as symptoms appeared while on antibiotics.
9:50 - Description of initial onset of disease.
14:30-19:00 Describes symptoms before doing the fecal transplant which include Fistula, fissures, hemmorhoids. Starting transplants on meds @ 40 mg prednisone recently at 80mg. explains all the medications he has tried during the course of his disease for IBD.
26:00 when and how he heard about fecal transplants
Video day#3-
Summary
1:25 bowel movement frequency reduced from 20X per day to around 2x per day, in about 5 days
Video Day #20
2:50 almost entirely off of medication at this point. he’s generally still doing very well bowel wise and feeling pretty good.
6:00 encourages people to try it, considers it a miracle for him and his condition.
Latest update April 30th, 2013-
0:00-3:30 gained 30 pounds since starting fecal transplants, eats a normal diet now and most symptoms are gone without medication.
3:30-7:32- tips on how to perform the transplant
Testimony #2-
His screen name is Dr. Briggs and he is a university physics professor who is trained as a scientist and who has done the treatment successfully at home using his wife as a donor.
link to the forum discussion where this testimony was found-
http://www.healingwell.com/community/default.aspx?f=38&m=2541306&p=4
summary- he has had ulcerative colitis for 12 years, then later was diagnosed with crohn’s disease. He suspects that a course of antibiotics had something to with him developing IBD.
symptoms before starting the Fecal transplant were 3 bm’s per day, previously he has had up to 20 per day. after the transplants he averaged 2 bms a day and he was able to eat foods that used to cause his symptoms to worsen, this indicates a major change occurred in his ability to digest food.
A few quotes from his fecal transplant experience-
posted on 11/27/2012
Dr Briggs-
“So, things are going very well. To recap - I was diagnosed with UC about 12 years ago, and spent time on sulfasalazine and prednisone with no benefit (15-20 bloody very loose stools a day), then eventually Remicade after developing a fistula. I was on the Remicade for a little over 7 years, which partially controlled things (5-7 loose stools a day, no bleeding as long as I got infusions every ~11 weeks).
I am now off all medications, and doing great. Two well-formed stools a day.”
Posted 2/28/2013 1:14 PM
Dr briggs- “Sorry for not responding sooner (a lot sooner) - with my UC seeming to be completely gone, I'm getting caught up in other things, so I have to remind myself to occasionally check out this thread.
Potatoes are often not well digested if you have a compromised GI system, they have lots of complex starches in them. I can eat them now without problems, but before the transplants they gave me issues - and early on after the transplants when I ate potatoes they would give me a very mushy stool afterwards (I have continued healing since the transplants, and now tolerate everything very well it seems - except wheat). “
Testimony# 3
Here is another testimony from a women with the screenname bustersmom, she avoided a colectomy by doing a fecal transplant at home using her husband as a donor-
link-http://www.crohnsforum.com/showthread.php?t=15548&highlight=bacteriotherapy
post# 139
I have Crohn's disease and was on Flagyl and Cipro for over two weeks and got three abscesses. I figured i had nothing to lose by trying the transplant. I waited three weeks after finishing the antibiotics and was in bad shape. abscesses were terrible. I did the transplant daily for a while and the abscesses, Two which were large, Began to shrink every day. After a month they were gone, and made NO fistula! I haven't had one bit of trouble down there since. I believe the transplants work. I don't know if it works all through the colon, but it worked on me in my lower colon and i was a complete mess. Bree
Testimony#4
"Last Fall I went to Sydney Australia on a vacation and while I was there I looked into their programs and research. I found FMT. Fecal Microbiota Transplantation. I was grossed out and said oh hell no. Still, the more I studied and read the more it seemed worth a try. So, I called my doctor here and asked if I could be in one of the clinical studies. Unfortunately there wasn't one here. Only in Portland Oregon. He happened to know the doctor running the study though and offered me another way to treat myself at home. My husbands stool was tested for HIV, Hep A B and C, C Diff, and he passed all the tests with flying colors. So, we bought a retention nozzle, enema bag, tons of Zip lock freezer bags, went through training with our nurses so he could help me complete the series of enemas and my flora was checked and measured by my doctor every other week 7 days after each treatment. I was really sore down there from all the surgeries so instead of 7 days of back to back enemas we changed it to once every other week for 2 months.
I felt it was my last hope and I wanted to try something because nothing else seemed to work and I just wanted to become a guinea pig if I could. 4 months after my (home treatment) I went in for a scope, except some scarring from the past issues I had no inflammation, no diarrhea, no pain, and had started to work out again. I have felt better this past year than I have since I was 26. I have my life back! I have not been on any meds for 6 mos and after my scope today I was told I was in complete remission. (They still don't know how long it may last or if it will.) Right now I feel normal, no pain, no D and I have energy again!"
source-
http://www.crohnsforum.com/showthread.php?t=48939
4. GENERAL INFO
Here are some general videos explaining how this treatment has potential for IBD and many other diseases. Various environmental toxins and even antibiotics are suspected to be involved in damaging intestinal bacteria, which may contribute to developing these conditions.
Video Interview of Professor Lawrence J. Brandt.
Here are some credentials/education: Chief Emeritus of Gastroenterology and Professor of Medicine and Surgery at the Albert Einstein College of Medicine. He also has been performing studies on fecal transplants in C difficile in the U.S. since about 1999. C difficile is very similar to Inflammatory Bowel disease which the mains symptoms are chronic diarrhea and often include colonic inflammation just like inflammatory bowel disease.
Link to verify Professor Brandt’s credentials
http://www.einstein.yu.edu/departme...gy-liver-diseases/faculty/profile.asp?id=2519
Part 1-
-talks about his experience studying fecal transplants for C. Difficile Infection.
Part 2-
http://www.youtube.com/watch?v=ot7e9bQO2U8
-his opinion on fecal transplant overall safety, and its potential for other diseases.
Part 3-
http://www.youtube.com/watch?NR=1&feature=endscreen&v=u8eNvAVfc0M
SUMMARY-
1:10 history of fecal transplant in veterinary medicine
2:18 different routes of administration of Fecal transplant
3:00 self/home administration of fecal transplant
4:00 more on the future and potential of Fecal Transplant
5:38 mentions pill form as the final future method of administration in the future for fecal transplant.
here is an article published on February 13, 2013 by Lawrence J. Brandt and another professional which was published in current opinion in gastroenterolology
Fecal Microbiota Transplantation: Past, Present and Future
Olga C. Aroniadis, Lawrence J. Brandt
Curr Opin Gastroenterol. 2013;29(1):79-84.
link to article-
http://www.medscape.com/viewarticle/776501_1
Video, By Cara Louise Santa Maria - Science educator, Masters
Degree in Neuroscience
link-
http://www.youtube.com/watch?feature=endscreen&NR=1&v=kLB5Pasjjis
Here is a very well written article On FMT by KSS , a member of this website. there are testimonies of people who have tried Fecal transplant in this article.
http://diyehr.com/analysis-of-crohn...e-peer-to-peer-observational-treatment-study/
Article for TIME magazine in June 2012 about microbiome research-
http://healthland.time.com/2012/06/14/the-good-bugs-how-the-germs-in-your-body-keep-you-healthy/
http://commonfund.nih.gov/hmp/overview
Dr. Martin Blaser has studied the role of bacteria in human disease for over 30 years. He is the director of the Human Microbiome Program at NYU. His new book was just published and discusses the new evidence suggesting antibiotics have contributing to rising rates of diseases like Crohn's by killing off good microbes. -
http://martinblaser.com/
http://www.npr.org/2014/04/14/302899093/modern-medicine-may-not-be-doing-your-microbiome-any-favors
http://www.amazon.com/gp/product/08...iveASIN=0805098100&linkCode=as2&tag=yoadsu-20
--------------------------------------------
5. How to Select a Donor
Overall, as long as the Donor is in good health, there is very little risk with doing a fecal transplant. Even in some of the documents below they reported bypassing blood tests and health screening for some patients who chose a donor that was a family member that they knew and trusted, buts it probably best to take precautions. All the criteria for selecting a healthy donor and directions for what blood tests they need were obtained from these two papers, one of which was written by doctor Borody and other professionals in the field.
Requirements:
NO ANTIBIOTICS IN LAST 6 MONTHS, OR EVER IS BEST.
NO Gastrointestinal COMPLAINTS LIKE FREQUENT DIARHEA OR CONSTIPATION/excessively firm stool that is hard to pass, blood, No Mucus in stool or intestinal pain. You should have a generally regular stool frequency of 1-2 bowel movements per day.
Absence of metabolic syndrome-
http://en.wikipedia.org/wiki/Metabolic_syndrome
Symptoms and features are:
-Fasting hyperglycemia — diabetes mellitus type 2 or impaired fasting glucose, impaired glucose tolerance, or insulin resistance
-High blood pressure
-Central obesity (also known as visceral, male-pattern or apple-shaped adiposity), overweight with fat deposits mainly around the waist
-Decreased HDL cholesterol
-Elevated triglycerides
Associated diseases and signs are: hyperuricemia, fatty liver (especially in concurrent obesity) progressing to NAFLD, polycystic ovarian syndrome (in women), and acanthosis nigricans.
No autoimmune conditions- list of conditions-
link-
http://womenshealth.gov/publications/our-publications/fact-sheet/autoimmune-diseases.cfm#d
No allergic diseases - asthma, atopic dermatitis (eczema), allergic rhinitis (hay fever), food allergies
Required Blood Tests for donors- full blood count, liver function,
Negative viral screening for HIV 1 and 2, Hepatitis a, b, c. cytomegalovirus, Epstein Barr Virus, Syphilis.
Some studies have bypassed donor screening only in cases where close family members have been selected as donors.
None of the Testimonys I listed in sections #4 of this paper mentioned taking the suggested precautions to follow the donor selection criteria, as most were able to get help from family members who they were confident were healthy. I plan on taking full precautions no matter how healthy my donor is, or whether they are a family member or not. I also have additional criteria that go beyond the advice listed here.
The papers below is where i found most of this information. It is not required that you read these papers with the web links listed below, but if you would like to look them up to verify they exist, feel free to do that.
Article 1
Details on page 3-
http://www.2ndchance.info/inflambowel-Hamilton2011.pdf
Article 2
Details on page 479-
http://www.cdd.com.au/pdf/publications/paper12.pdf
Recommended diet for donors- this will encourage all the good bacteria in your intestine to grow and make it a more potent medicine.
High fiber foods, like whole grain oats and wheat
Berries.
eat at least one apple per day.
veggies.
if you smoke, reduce your smoking as much as possible.
Things to avoid- anything with aspartame or saccharin in it, excessive meat. excessive amounts of processed food in packaging as it may contain preservatives that inhibit bacterial growth.
over consumption of meat- beyond 8 ounces in a day would be excessive.
other tips-
if you become sick or get food poisoning while doing the transplants you will have to stop until you become better.
--------------------------
6. How To perform a Fecal Transplant
chapter a work in progress
RECTAL METHOD/BY ENEMA
I have not included yet any details on how the transplant is done in any precise way, but typically it is done by making a solution of saline (.9% sodium chloride solution/aka salt water) mixed with stool in a blender and giving it as an enema to retain in the body for 6-8 hours or as long as your body can hold it. I will add more very soon but i think it's all here if you want to figure out the details for yourself, otherwise i will soon give some better instructions to make it easy for people to try themselves. There are some details on page 5 and 6 of this paper by doctor borody.
http://www.cdd.com.au/pdf/publications/paper12.pdf
how to make saline solution at home-Quick instructions- mix one gallon of distilled water with 4 teaspoons of salt(preferablly pharma grade neti pot salt) in a pot and stir on low heat so salt easily dissolves. this will make a gallon of saline solution.
.9% sodium chloride w/v solution is expressed as a mass concentration weight/volume solution. in other words, it is telling us how much mass of a certain substance is dissolved within a volume of a fluid. in this case, 100 milliliters of a fluid. and in this case sodium chloride aka salt. So there is .9 grams(just shy of one full gram) of salt dissolved in every 100 milliliters of h20 aka water.
more to come...

 journals.plos.org
journals.plos.org



















/cloudfront-eu-central-1.images.arcpublishing.com/prisa/JEUHBGFU6FA5PLNTMVRJAEWXV4.jpg)