I know Dusty has agreed with me before (I wasn't sure until she said so! :lol

but, you will KNOW it's not in his lungs! If it was, he would be gagging, coughing, etc. I think the question about the lungs is more crucial when you're dealing with infants or those unable to respond as well as C would.
We maybe became very complacent

but S stopped checking the PH level after a little while, although he did continue to check for stomach fluid (but, even this, sometimes came up empty??). Side note - do not let C drink red gatorade before checking stomach fluid!!! Gave S and I quite a scare once until he remembered about the gatorade! The stethoscope was hard to 'hear' and, I'm assuming you're listening for the 'pop'??? If yes, when you push the air in, make sure you push the air in quickly... slowly won't give you the pop sound. Easier when two people do it - one pushing the plunger, the other listening...
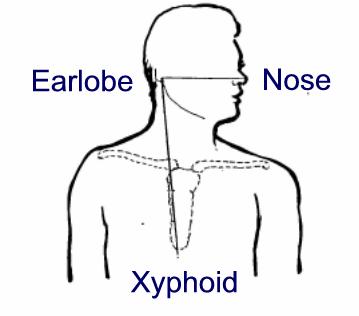
Did you guys measure the tube? If I remember correctly, to find the right measurement you do:
(Measure this outside his body) Put the end of the tube (the part the will end up in his stomach) about 3 finger widths below his sternum (might be a bit more if he's tall??:confused2

, from there the tube should run up his chest, up behind his ear, across his cheek and to his nostril. The point where it reaches his nostril will be how far it needs to be inserted. I don't know if this is helpful S's tubes had numbers on it and his measurement on S's was approx. 60 (but, I don't know if the numbers represented inches or if they vary by manufacturer). Once you have this measurement, mark it with a marker because this will always be how far he needs to insert it. To make it even easier for him, at that mark, cut some tape about 1-2 mm thick and wrap at that point - when he's inserting the tube, he doesn't need to worry about 'watching' for the right spot, he'll feel the tape.
Did they give C some lubricating and/or numbing gel? S used it at the beginning and it helps the tube slide down easier. Also, is he drinking water as he's inserting the tube?
I hope all that made sense!!
(Dusty - confirmation I'm give 'safe' advice is always helpful! :lol2